Small animal veterinary case study – Lucy the DSH cat
Case provided by Yvonne McGrotty BVMS CertSAM DipECVIM-CA MRCVS
European Specialist in Veterinary Internal Medicine
RCVS Specialist in Veterinary Internal Medicine
History:
Lucy, a 5yr FN DSH, was presented with a recent history of weight loss despite increased appetite. Bloods revealed azotaemia with hyperphosphataemia. Haematuria was also noted along with a mild non-regenerative anaemia.

Previous history included the removal of bladder stones in 2013 which were confirmed to be calcium oxalate.
Physical Examination:
On clinical examination Lucy was bright and alert and in reasonable body condition at 2.9kg. Thoracic auscultation was complicated by purring but there was a suspicion of a gallop rhythm. Pulse quality was reduced. There was no obvious pain on abdominal palpation. A goitre was not identified. Blood pressure was on the low side at 110mmHg systolic.
Clinical Pathology:
Venous blood gases revealed a fully compensated metabolic acidosis with increased anion gap consistent with uraemia. Ionised calcium was significantly increased. PTH was within reference range and PTHrP was unremarkable so the hypercalcaemia is likely to be idiopathic.
Diagnostic Imaging:
Following sedation, an abdominal ultrasound was performed focussed on the urinary tract. Both kidneys contained echogenic regions with distal shadowing consistent with renoliths (Figure 1). There was no evidence of hydronephrosis or hydroureter but both kidneys did show decreased cortical blood flow and increased cortical echogenicity. The urinary bladder revealed a focal change cranially which may reflect a scar from the site of the previous cystotomy. There was no evidence of bladder stones.
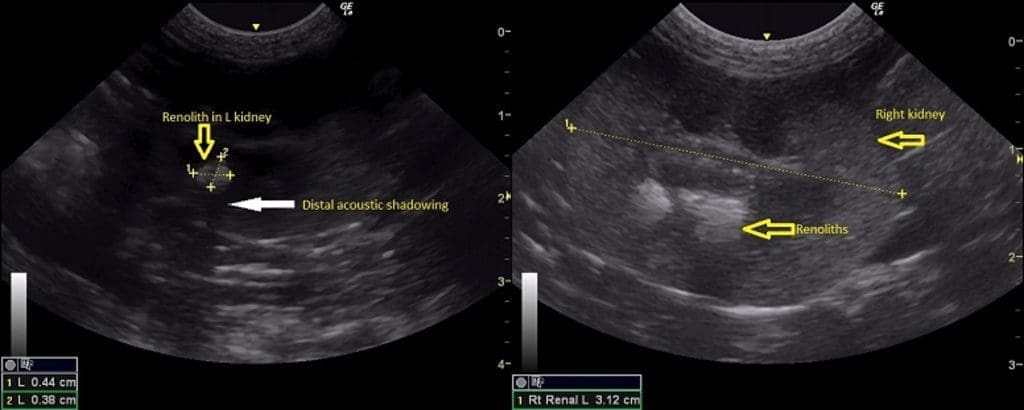
Figure 1. Ultrasound images of the left kidney (left) and right kidney (right). In both kidneys there is mineralised material (yellow arrows) with distal acoustic shadowing (white arrow).
A cystocentesis sample was collected and contained 2+ blood and 2+ protein. Urine SG was 1.020 prior to fluid therapy confirming that the azotaemia is renal in origin. Sediment examination confirmed the presence of red and white cells and culture was positive (E. coli) consistent with a bacterial UTI.
Lateral and DV abdominal radiographs were obtained which confirmed that Lucy has fairly sizeable bilateral renoliths (Figure 2). It would seem likely that these are calcium oxalate given previous history and presence of hypercalcaemia. A Bates body which is thought to occur due to fat necrosis was also noted incidentally.
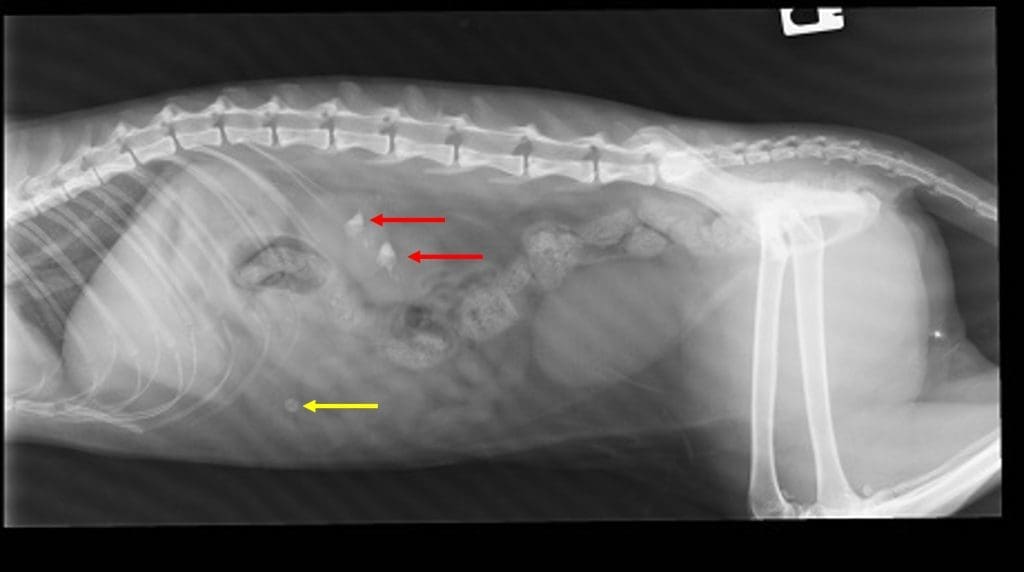
Figure 2. A right lateral abdominal radiograph. Radiopaque renoliths are visible within the collecting system of both kidneys (red arrows). The incidental fat necrosis appears as a round radiopaque area within the ventral abdomen (yellow arrow).
Diagnosis:
IRIS stage 3/4 non-hypertensive renal failure with bilateral renoliths and idiopathic hypercalcaemia